Dosage
Depressive Disorder
Once a day. The usual dose is 10 mg daily, and the maximum daily dose may be increased to 20 mg based on individual patient response. Antidepressant effects are usually achieved in 2-4 weeks. After symptoms are relieved, treatment should be continued for at least 6 months to consolidate the effect.
Panic disorder with or without agoraphobia
Once a day. The recommended starting dose is 5 mg per day, which can be increased to 10 mg per day after 1 week. Depending on the patient’s individual response, the dose can be further increased to a maximum dose of 20 mg per day.
The best effect can be achieved after treatment for about 3 months. Treatment usually lasts several months.
Elderly patient (65 years old)
It is recommended to start treatment with half the usual starting dose mentioned above, and the maximum dose should be reduced accordingly.
Children and young people ([18 years old])
This product is not suitable for children and adolescents under 18 years of age.
Those with reduced kidney function
Patients with mild to moderate renal function reduction do not need to adjust the dose, and patients with severe renal function impairment (CLcr [30 mL/min]) should use with caution.
Those with reduced liver function
The recommended starting dose is 5 mg daily and continued treatment for 2 weeks. Based on individual patient response, the dose may be increased to 10 mg daily. Caution and particularly cautious dose increases are recommended in patients with severely reduced hepatic function.
Cytochrome P450 2C (CYP2C19) slow metabolizers
For patients known to be poor metabolizers of CYP 2C19, the recommended starting dose is 5 mg daily for 2 weeks. Based on individual patient response, the dose may be increased to 10 mg daily.
Drug withdrawal symptoms: Abrupt discontinuation of medication should be avoided. When treatment with this product needs to be stopped, the dose should be gradually reduced within 1-2 weeks to avoid withdrawal symptoms.
The safety of doses above 20 mg daily has not been established.
Taboo
1. People who are allergic to the active ingredients or any excipients of this product are prohibited from using it.
2. Do not use it in combination with non-selective, irreversible monoamine oxidase inhibitors (MAOIs).
3. Combination use with linezolid is prohibited.
4. It is prohibited to take this drug in combination with pimozide.
5. This product is contraindicated in patients with known QT prolongation or congenital QT syndrome.
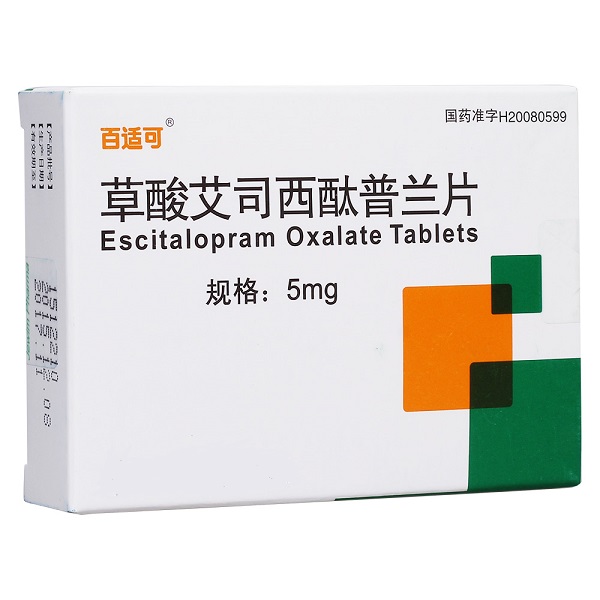
[Picture]
Notes
The following special warnings and cautions apply to all types of SSRI drugs.
Ambivalent anxiety
Some patients with panic disorder may experience aggravation of anxiety symptoms in the early stages of antidepressant treatment. This paradoxical reaction usually gradually reduces within 2 weeks after the start of treatment. It is recommended that lower starting doses may reduce this anxiogenic effect of the drug.
Epileptic seizure
Patients who experience a first seizure or who have been previously diagnosed with epilepsy should discontinue use of this product if the frequency of seizures increases. SSRIs should be avoided in patients with unstable seizures, and patients with controlled seizures should be monitored during treatment.
Mania
SSRI drugs should be used with caution in patients with a history of manic or hypomanic episodes. Patients who develop a manic episode should discontinue SSRIs.
Diabetes
For patients with diabetes, treatment with SSRI drugs may affect blood sugar regulation. Patients taking insulin and/or oral hypoglycemic agents may require dosage adjustments of these medications.
Suicide, suicidal ideation, or worsening illness
Symptoms inherent in depression may include suicide attempts, self-injury, and suicide (suicide-related events), and may persist until significant improvement occurs as a result of treatment. Because improvement may not occur during the first few weeks of treatment or for several weeks thereafter, patients taking antidepressants should be monitored closely until their disease improves. Clinical experience generally suggests that the risk of suicide may be increased during the early stages of recovery. Other psychiatric events that occur with the use of this product are also associated with an increased risk of suicide-related events. In addition, psychiatric events may coexist with depressive disorders. Such precautions should also be taken when treating other psychiatric disorders that accompany depression. Patients who have had a suicide-related event or severe suicidal ideation prior to treatment with this product are known to be at greater risk for suicidal ideation or suicide attempts and should be carefully monitored during treatment. A meta-analysis of antidepressant and placebo-controlled studies in adults with depressive disorders showed that among patients under 25 years of age, those treated with antidepressants were at increased risk for suicidal behavior compared with those treated with placebo. Patients should be monitored closely during antidepressant therapy, especially in patients at high risk or during early treatment and dose adjustment periods.
Patients (and their caregivers) should monitor closely for any clinical deterioration, suicidal behavior or ideation, and unusual changes in behavior and seek immediate medical advice if these symptoms occur.
akathisia/psychomotor dysphoria
The use of SSRIs/SNRIs has been associated with the development of akathisia, which is characterized by unwilling or painful restlessness in subjects, the need to move frequently, and the inability to sit or stand quietly. Akathisia mostly occurs during the first few weeks of treatment. If a patient develops these symptoms, continuing to increase the dose may be harmful.
Hyponatremia
Hyponatremia is rarely seen with SSRIs (possibly due to anti-The efficacy was better than the usual starting dose of 10 mg.
In a 24-week long-term double-blind trial, the 10 mg escitalopram group and the 20 mg citalopram group were equally effective, and half of the patients in the escitalopram group withdrew due to adverse reactions. test. In a long-term trial of relapse prevention, 274 patients who responded to the treatment were randomized to receive the same dose of escitalopram or placebo after 8 weeks of open-label treatment with escitalopram 10 or 20 mg/day. 36 weeks. In the 36-week study, patients who received escitalopram experienced relapse significantly later than those who received placebo.
Panic disorder
In a 10-week controlled trial for the treatment of panic disorder, escitalopram at 5-20 mg/day was compared with placebo and citalopram at 10-40 mg/day. Efficacy of citalopram. By evaluating the frequency, severity, duration, accompanying symptoms and other indicators of panic attacks, it was shown that the escitalopram group had a significant statistical advantage in efficacy over the placebo group. Most treatment-related adverse events (≥5% of patients) were higher in the citalopram group than in the escitalopram group.
Social anxiety disorder
Three short-term (12-week) studies and one 6-month relapse prevention study showed that escitalopram was effective in patients with social anxiety disorder.
A 24-week long-term, placebo-controlled trial demonstrated the effectiveness of escitalopram at doses of 5, 10, and 20 mg.
The efficacy of escitalopram 20 mg/day in the treatment of social anxiety disorder is statistically superior to paroxetine 20 mg/day, escitalopram 5 mg/day and 10 mg/day. Transient withdrawal symptoms (lasting no more than 2 weeks in all active treatment groups) were observed in all treatment groups and were more pronounced in the paroxetine group relative to the escitalopram group (P≤0.05).
A pooled analysis including 670 escitalopram patients and 341 placebo patients showed that the effective rates were 58.1% and 40.2% (CGI-I score 1 or 2), respectively, and the recovery rates were 24.8% and 12.9% (CGI-S score 1 or 2) (P≤0.001).
Generalized anxiety disorder
The results of four placebo-controlled trials confirmed the effectiveness of escitalopram 10 mg/day and 20 mg/day, but not 5 mg/day.
A combined analysis from three 8-week clinical trials with similar regimens showed that among 421 patients treated with escitalopram and 419 patients treated with placebo, the effective rates were 47.5% and 28.9%, respectively (CGI- I score 1 or 2), the recovery rates were 37.1% and 20.8% (CGI-S score 1 or 2, P≤0.001). Sustained effects begin in the first week.
In four 12-week trials compared with paroxetine, escitalopram 10 mg/day was statistically significantly more effective than paroxetine 20 mg/day. Transient withdrawal symptoms were observed in both groups, and were more pronounced in the paroxetine group compared with the escitalopram group at doses of 5 mg, 10 mg, and 20 mg/day (P≤0.01).
A 24- to 76-week randomized, ongoing trial was conducted on 373 patients who responded to open therapy during the first 12 weeks. The risk of relapse was significantly reduced in patients treated with 20 mg/day of escitalopram.
Pharmacological effects
Escitalopram is the mono-S-enantiomer of the bicyclic hydrogenated phthalide derivative citalopram. The mechanism of escitalopram’s antidepressant effect may be related to inhibiting the reuptake of 5-HT by neurons in the central nervous system, thereby enhancing the function of central serotonergic nerves. In vitro and animal tests show that escitalopram is a highly selective 5-HT reuptake inhibitor (SSRI), which has little effect on the reuptake of norepinephrine and dopamine. Escitalopram is at least 100 times more active than the R-enantiomer in inhibiting 5-HT reuptake. No drug resistance was found in the long-term (up to 5 weeks) administration of escitalopram in the rat depression model.
Escitalopram has no affinity for 5-HT1-7 receptors, α receptors, β receptors, D1-5 receptors, H1-3 receptors, M1-5 receptors, and benzodiazepine receptors. , or simply have lower affinity. Escitalopram has no affinity for Na+, K+, Cl-, and Ca2+ channels, or only has low affinity.

 微信扫一扫打赏
微信扫一扫打赏

